Improving Healthcare Access for Mothers in Rural Texas
Overview
The Rural Texas Maternal Health Assembly includes diverse stakeholders, rural healthcare providers and administrators, senior officials from key state entities, and representatives from advisory committees. Selected members of the Assembly serve as a Working Group to delve deeper into the key issues identified through a survey of all Assembly members. To date, 38 Assembly members have responded to this survey to identify key issues and potential solutions for Texas mothers. Potential solutions and policy recommendations will be discussed during an in-person Assembly meeting in Austin, TX on September 6, 2024. The Rural Texas Maternal Health Assembly work group will finalize a Position Paper with comprehensive solutions and recommendations after this in-person meeting in Austin, TX. The final Position Paper with actionable policy recommendations for Texas will be published in mid-October.
On March 1, 2024, Texas implemented House Bill 12, extending Medicaid postpartum coverage to 12 months. Despite this progress, rural Texas mothers still face significant healthcare barriers.
On July 25, 2024, the Rural Texas Maternal Health Assembly was convened to address healthcare access obstacles and key issues faced by Texas mothers and rural providers in Texas.
A comprehensive Position Paper, developed by this diverse Assembly of healthcare experts, aims to address these challenges and propose actionable solutions for Texas.
Overview & Goals
The Purpose of this Assembly
To gather experts (rural providers, consumers, health plans, academic institutions, and foundations) focused on rural health in order to inform policy recommendations.
To understand the obstacles faced by mothers and providers and craft pragmatic interventions and recommendations regarding rural maternal health for the 89th Texas legislative session.

The Problem
Texas mothers in rural areas face significant barriers to accessing timely medical care and social services throughout their pregnancies. Nearly 50 percent of Texas counties lack obstetrical care clinicians or hospitals.
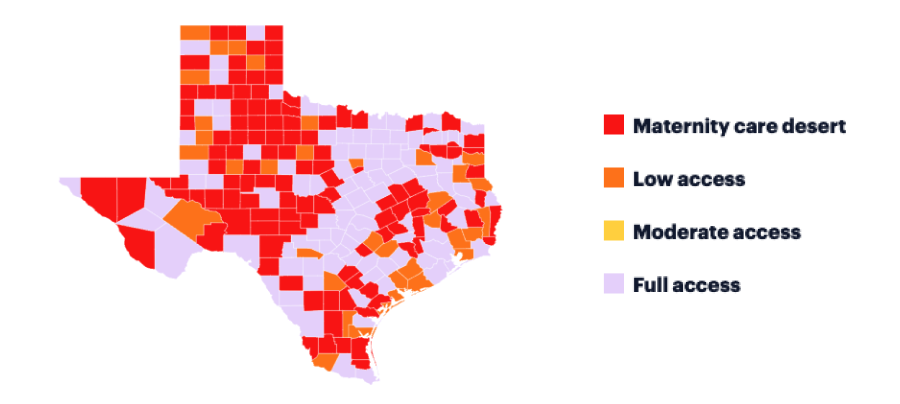
Source: March of Dimes
The Process
To address these issues, we have convened a Rural Texas Maternal Health Assembly in order to develop comprehensive rural maternal health recommendations and reforms.

Final Product
A Working Group is formed to delve deeper into key issues and solutions during an in-person meeting in Austin on September 6, 2024.
This Work Group will finalize a Position Paper with comprehensive solutions and policy recommendations for Texas. The final Position Paper will be published and widely disseminated in mid-October.

Participants
Assembly Conveners


Assembly Supporters

















Subject Matter Experts and Contributors



State Agency Information Resources



Advisory Entity Informational Resources

Co-conveners
Kia Parsi, MD
Executive Director
Texas A&M Rural and Community Health Institute
Texas A&M University Health Science Center
Lead Convener
Angie Alaniz, BA
Director of Operations
Texas A&M Rural and Community Health Institute
Texas A&M University Health Science Center
Lead Convener
Tom Banning
Texas Academy of Family Physicians
Co-Convener
Jacquelyn Alvarado, DNP, APRN, CNM, C-EFM
Maternal Fetal Focus Program Manager
Texas A&M Rural and Community Health Institute
Texas A&M University Health Science Center
Lead Convener
Ankit Sanghavi
Executive Director Texas Health Institute
Co-Convener
John Henderson
CEO/Executive Director Texas Organization
of Rural and Community Hospitals
Co-Convener
Assembly Timeline
Participant Timeline
Assembly kick-off meeting
July 25th 12pm, 2024
Survey Completed
38 Experts participated in the survey
47 Assembly members participated in this process
Key Expert Interviews
Month of July and August, 2024
Work Group development of draft position paper
August, 2024
Maternal Health Assembly Work Group
September 6, 2024 (Austin)
Circulate position paper
September, 2024
Publication of the position paper
October 25th, 2024
Contact
Bita Kash, PhD, MBA, FACHE
Texas A&M Rural and Community Health Institute
Consultant
dropthebita@gmail.com
Helen Kent Davis, Senior Advisor
Texas Academy of Family Physicians
Texas Health Institute
Consultant
helen@hkdhealthpolicy.com
Additional Resources
Models to explore
Rural OB Access & Maternal Services (ROAMS) in NM
State Perinatal Quality Collaboratives – CDC Division of Reproductive Health: Texas Collaborative for Healthy Mothers and Babies
Medicaid reimbursement for non-clinical services such as meals, doulas and other SDOH services
CHW and Navigator programs – HRSA Maternal & Child Health (MCH) Navigator
Kansas recruits rural docs in medical school and pays for their tuition if they serve 4 years after residency
The Centering Model has been implemented across the US in an effort to improve maternal/neonatal outcomes
Tandem Teen Prenatal and Parenting Program Mobile Units and home visiting programs
Rural Maternal Health Resources
Background Materials/Data Resources
Texas Health Data - Maternal Health2022-MMMRC-DSHS-Joint-Biennial-Report.pdf (texas.gov)
Maternal Health: Availability of Hospital-Based Obstetric Care in Rural Areas | U.S. GAO
TCHMB
2024 State Scorecard on Women’s Health and Reproductive Care | Commonwealth Fund
State Policy Lever Checklists - Prenatal-to-3 Policy Impact Center (pn3policy.org)
A Worsening Crisis: Obstetric Care in Rural America (harvard.edu)
U.S. maternal health: State shares of rural hospitals without maternity care (axios.com)
HRSA Invests Nearly $90 Million to Address Maternal Health Crisis | HRSA
Creating Health Care Models to Improve Maternal Health | MCHB (hrsa.gov) (Bexar county hospital district received funding)
Task Force on Maternal Mental Health National Strategy to Improve Maternal Mental Health Care (samhsa.gov)
Maternity Care Access
Can Family Doctors Deliver Rural America From Its Maternal Health Crisis? - KFF Health News
Where You Live Matters: Maternity Care Deserts and the Crisis of Access and Equity | March of Dimes
Maternal Health in Rural Communities
Rural Obstetric Unit Closures - The University of Minnesota Rural Health Research Center (umn.edu)
Restoring Access to Maternity Care in Rural America | Commonwealth Fund
Postpartum Morbidity and Mortality and Health Care Utilization in Rural vs. Urban Communities - The University of Minnesota Rural Health Research Center (umn.edu)
Microsoft PowerPoint - Hospital Webinar FINAL (nationalacademies.org)
Rural resilience: The role of birth centers in the United States - Jolles - 2020 - Birth - Wiley Online Library
Promoting Safety in Community-Based Birth Settings | AAFP
Assessment of interprofessional collaboration at free-standing birth centers: Does collaboration influence outcomes? - ScienceDirect
Postpartum Newborn Home Visits | SCDHEC
Racial Disparities in Maternal and Infant Health: Current Status and Efforts to Address Them | KFF
Innovation
HRSA Administrator Carole Johnson, Joined by Rep. Lauren Underwood, Launches New National Maternal Health Initiative | HRSARural Maternal Health Toolkit - RHIhub (ruralhealthinfo.org)
HRSA Rural Maternal Health Initiatives - RHIhub Webinar (ruralhealthinfo.org)
Rural Maternal Health – Models and Innovations - Rural Health Information Hub
Expanding Telehealth for Improved Maternal Outcomes - Maternal Health Learning and Innovation Center
Maternal Opioid Misuse (MOM) Model | CMS
rural-case-study-meeting-essential-health-services-and-reimagining-obstetrics-in-a-rural-community-rural-case-study-april-2024.pdf (aha.org)
Postpartum Primary Care Engagement Using Default Scheduling and Tailored Messaging: A Randomized Clinical Trial | Public Health | JAMA Network Open | JAMA Network
Maternity Care Payment Reform | National Partnership for Women & Families
Blueprint for Advancing High-Value Maternity Care Through Physiologic Childbearing | National Partnership for Women & Families
Postpartum Discharge Transition Staging | AIM (saferbirth.org)
Community-Based Models Improve Maternal Outcomes and Equity | Commonwealth Fund
Navigating geographical disparities: access to obstetric hospitals in maternity care deserts and across the United States | BMC Pregnancy and Childbirth | Full Text (biomedcentral.com)
Improving access to maternal care in rural communities | AHA News
Mapped: Over half of rural hospitals don't offer maternity care (advisory.com)
Proposed Solutions for Improving Maternal Health Care in Rural America - PubMed (nih.gov)
The Role of the Family Physician in Rural Maternity Care
CNM/CMs Fill the Gap in Rural Maternal Care
The Need for Reliable Robust Maternal Transport Program to Improve Maternal Outcomes in Rural America
Text And Telephone Screening And Referral Improved Detection And Treatment Of Maternal Mental Health Conditions | Health Affairs
Mental Health Conditions Increase Severe Maternal Morbidity By 50 Percent And Cost $102 Million Yearly In The United States | Health Affairs
Centering Healthcare Institute | CenteringPregnancy
Medicaid-Payment-Initiatives-to-Improve-Maternal-and-Birth-Outcomes.pdf (macpac.gov)
Chapter 4: Maternity Care (hcp-lan.org)
Preventive/Primary Care
Access to and Use of Midwifery Care for Rural Residents - The University of Minnesota Rural Health Research Center (umn.edu)New Recommendations for Number of Required Prenatal Visits - The ObG Project
A Toolkit for Implementing Two-Generation Postpartum Care - I PROMOTE-IL (ipromoteil.org)
UMN-Case-Series_Postpartum-Support_8.4-final.pdf
MiPath Infographic for Providers (acog.org)
Telemedicine in Low-Risk Obstetrics - ScienceDirect
Obstetrics & Gynecology (lww.com)
Postpartum care needs assessment: women’s understanding of postpartum care, practices, barriers, and educational needs | BMC Pregnancy and Childbirth | Full Text (biomedcentral.com)
Provider Perspectives on Barriers and Facilitators to Postpartum Care for Low-Income Individuals - PMC (nih.gov)
NMDOH
Food Insecurity, Chronic Disease, and Health Among Working-Age Adults (usda.gov)Getting around rural America without a car is hard. These communities developed solutions | KCUR - Kansas City news and NPR
Rural Hunger and Access to Healthy Food Overview - Rural Health Information Hub
Food Insecurity in the Rural United States: An Examination of Struggles and Coping Mechanisms to Feed a Family among Households with a Low-Income - PMC (nih.gov)
Systematic Review of Interventions Addressing Food Insecurity in Pregnant Women and New Mothers - PMC (nih.gov)
Food Insecurity and Cardiovascular Health in Pregnant Women: Results From the Food for Families Program, Chelsea, Massachusetts, 2013–2015 (cdc.gov)
Pregnant and hungry: addressing food insecurity in pregnant women during the COVID-19 pandemic in the United States - PMC (nih.gov)
Food insecurity among pregnant women living in high-income countries: a systematic review - The Lancet
Relevant Peer-Reviewed Papers Published since 2020
Ahn, R., Gonzalez, G. P., Anderson, B., Vladutiu, C. J., Fowler, E. R., & Manning, L. (2020). Initiatives to reduce maternal mortality and severe maternal morbidity in the United States: A narrative review. Annals of Internal Medicine, 173(11_Supplement), S3-S10. https://www.acpjournals.org/doi/full/10.7326/M19-3258Singh, G. K. (2021). Trends and social inequalities in maternal mortality in the United States, 1969-2018. International Journal of Maternal and Child Health and AIDS, 10(1), 29. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7792749/
Chinn, J. J., Eisenberg, E., Dickerson, S. A., King, R. B., Chakhtoura, N., Lim, I. A. L., ... & Bianchi, D. W. (2020). Maternal mortality in the United States: research gaps, opportunities, and priorities. American journal of obstetrics and gynecology, 223(4), 486-492. https://www.sciencedirect.com/science/article/abs/pii/S0002937820307420
Ziller, E., & Milkowski, C. (2020). A century later: Rural public health’s enduring challenges and opportunities. American journal of public health, 110(11), 1678-1686. https://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2020.305868
Kozhimannil, K. B., Interrante, J. D., Tuttle, M. K., & Henning-Smith, C. (2020). Changes in hospital-based obstetric services in rural US counties, 2014-2018. Jama, 324(2), 197-199. https://jamanetwork.com/journals/jama/article-abstract/2768124
Leider, J. P., Meit, M., McCullough, J. M., Resnick, B., Dekker, D., Alfonso, Y. N., & Bishai, D. (2020). The state of rural public health: enduring needs in a new decade. American journal of public health, 110(9), 1283-1290. https://ajph.aphapublications.org/doi/full/10.2105/AJPH.2020.305728
Mehta, L. S., Sharma, G., Creanga, A. A., Hameed, A. B., Hollier, L. M., Johnson, J. C., ... & American Heart Association Advocacy Coordinating Committee. (2021). Call to action: maternal health and saving mothers: a policy statement from the American Heart Association. Circulation, 144(15), e251-e269. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001000
Shah, L. M., Varma, B., Nasir, K., Walsh, M. N., Blumenthal, R. S., Mehta, L. S., & Sharma, G. (2021). Reducing disparities in adverse pregnancy outcomes in the United States. American heart journal, 242, 92-102. https://www.sciencedirect.com/science/article/abs/pii/S0002870321002258?via%3Dihub
Merkt, P. T., Kramer, M. R., Goodman, D. A., Brantley, M. D., Barrera, C. M., Eckhaus, L., & Petersen, E. E. (2021). Urban-rural differences in pregnancy-related deaths, United States, 2011–2016. American journal of obstetrics and gynecology, 225(2), 183-e1. https://www.ajog.org/article/S0002-9378(21)00144-7/abstract